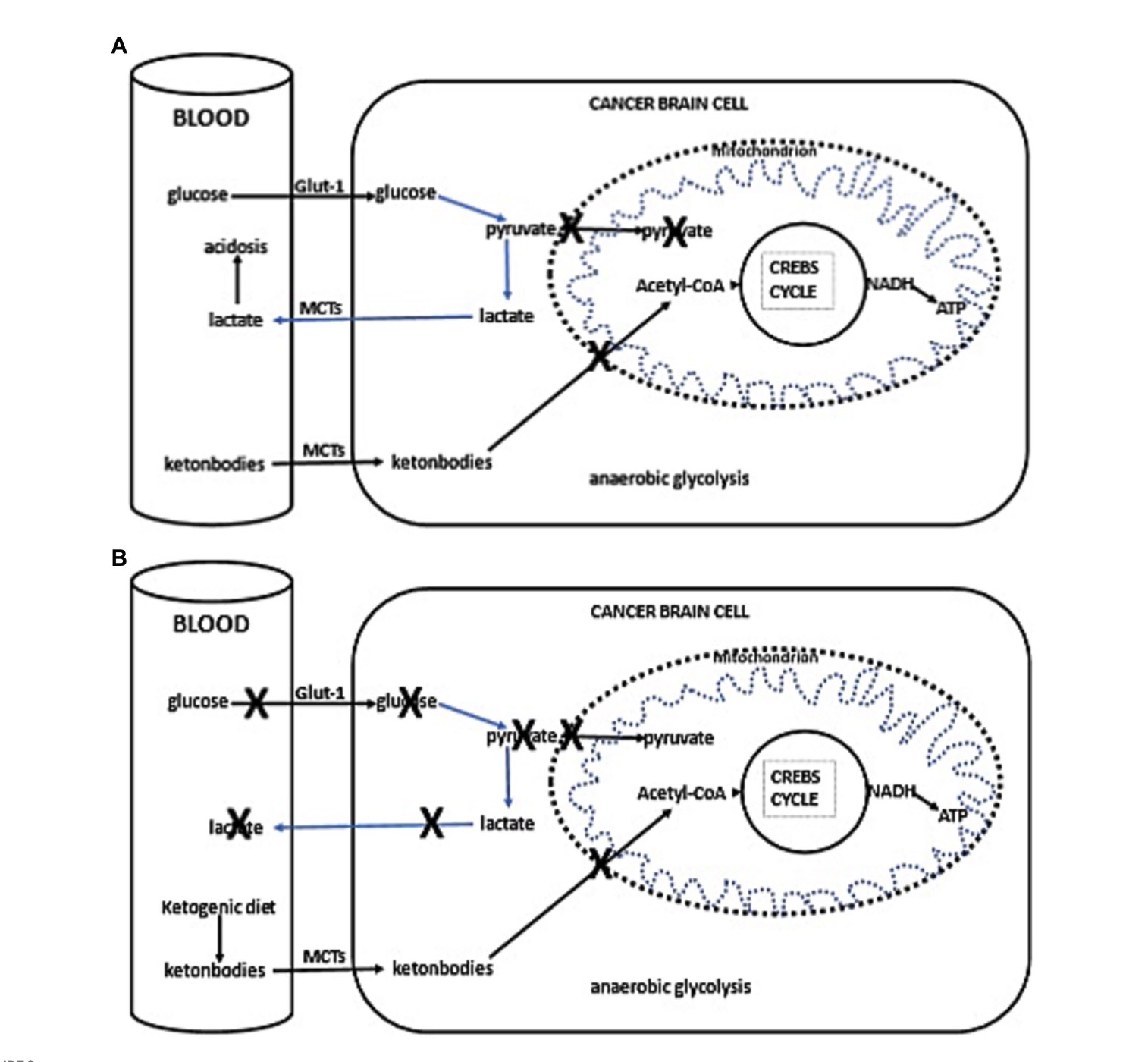
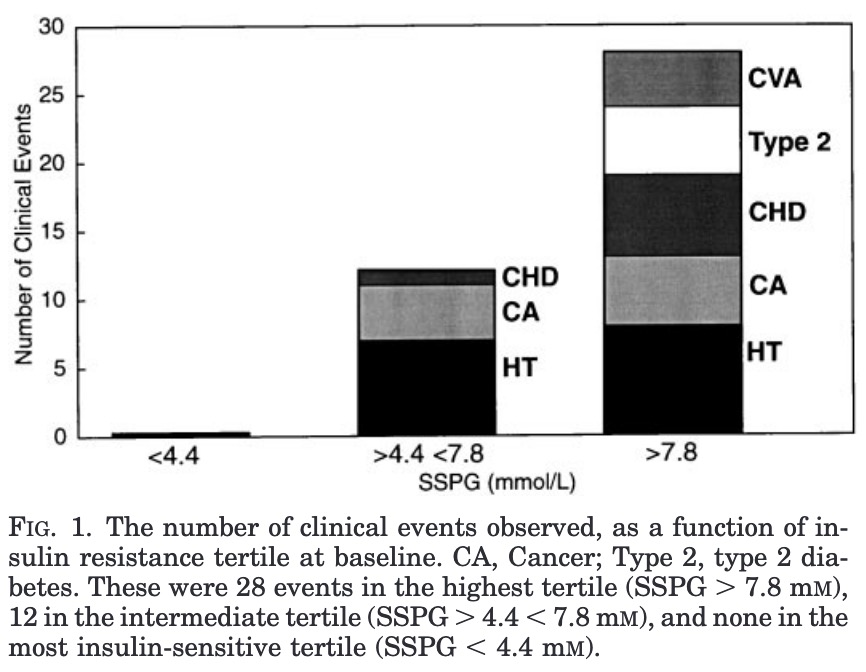
Otto Warburg originally proposed that cancer arose from a two-step process. The first step involved a chronic insufficiency of mitochondrial oxidative phosphorylation (OxPhos), while the second step involved a protracted compensatory energy synthesis through lactic acid fermentation. His extensive findings showed that oxygen consumption was lower while lactate production was higher in cancerous tissues than in non-cancerous tissues. Warburg considered both oxygen consumption and extracellular lactate as accurate markers for ATP production through OxPhos and glycolysis, respectively. Warburg’s hypothesis was challenged from findings showing that oxygen consumption remained high in some cancer cells despite the elevated production of lactate suggesting that OxPhos was largely unimpaired. New information indicates that neither oxygen consumption nor lactate production are accurate surrogates for quantification of ATP production in cancer cells. Warburg also did not know that a significant amount of ATP could come from glutamine-driven mitochondrial substrate level phosphorylation in the glutaminolysis pathway with succinate produced as end product, thus confounding the linkage of oxygen consumption to the origin of ATP production within mitochondria. Moreover, new information shows that cytoplasmic lipid droplets and elevated aerobic lactic acid fermentation are both biomarkers for OxPhos insufficiency. Warburg’s original hypothesis can now be linked to a more complete understanding of how OxPhos insufficiency underlies dysregulated cancer cell growth. These findings can also address several questionable assumptions regarding the origin of cancer thus allowing the field to advance with more effective therapeutic strategies for a less toxic metabolic management and prevention of cancer.
Full Paper https://doi.org/10.1007/s10863-025-10059-w